Written by
Dr Claire Farrow, Specialist Clinical Psychologist, (previously Trainee Clinical Psychologist on the Doctorate in Clinical Psychology course), Centre of Applied Psychological Sciences, Pain and Long Term Conditions Theme, email: clairefarrow@nhs.net
The following study was completed in partial fulfilment of the Doctorate in Clinical Psychology Course at Teesside University.
The World Health Organisation (WHO, 2016) categorise neurological conditions as disorders of the central and peripheral nervous system. Their definition includes epilepsy, stroke, multiple sclerosis (MS), Parkinson’s disease, and brain trauma. There is an increase in the likelihood of mental health conditions in those with neurological conditions. Depression is a common comorbidity (up to 50%), as well as an association with breakdown of relationships, unemployment and suicidality (Hind et al., 2014).
Acceptance and Commitment Therapy (ACT) is an intervention that uses mindfulness and acceptance strategies to foster a pursuit of a more value-based life. ACT has shown promising evidence of its utility for the neurological group (Graham et al., 2014; 2016; Kangas & McDonald, 2011). It aims to challenge avoidance strategies and increase the engagement of meaningful activity (Dindo et al., 2017). The therapy takes the stance that pain, grief and loss are a normal part of life (Harris, 2009).
Interpretative Phenomenological Analysis (IPA) was used as the interpretation method for semi structure interviews with participants. It is a qualitative method of analysis developed by Smith et al., (2013), concerned with the detailed examination of the human lived experience. Nine participants were recruited from two community Neuropsychology services across the North East, with a range of diagnoses including Multiple Sclerosis, Traumatic Brain Injury and stroke. Participants varied across the lifespan and there were five males and four female.
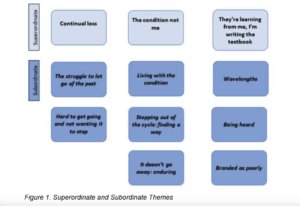
Figure 1. illustrates the themes developed by the analysis. Themes demonstrated the loss felt by participants, the struggle of illness, and the importance of knowing you are not alone in this situation. This is especially prominent due to the perceived stigma that is faced by those with neurological conditions. It was also identified that there is an ongoing clinical need for those with neurological conditions to engage in therapy. The idea of short term, one off therapy is not enough for those with such complex conditions. Participants identified that they were often left with a “wondering” of “what next” as well as having to tolerate the uncertainty of health.
ACT takes the approach of not attempting to remove or reduce the existence of distress, but aids people to live their best lives alongside their condition. The research highlighted the role of validation and acceptance by others. It was evident from the current research that the participants not only face stigma from society, but also face incredible isolation from others, especially within the neurological conditions population. Therefore it is essential within the therapeutic setting that individuals feel accepted and connected to others. Consequently, there is an identified role for psychology in terms of staff training around ensuring service users feels validated in their experiences and are given the opportunity to be heard.
The project was initially undertaken due to a limited evidence base for ACT. It was not expected to have such a profound effect upon practice and thinking. It has led to greater understanding around the loss felt by those experiencing significant health events, in terms of identity, role, purpose, and sense of self. It is important for clinicians working within such neurological settings to consider the impact of loss, and the wider stigma from society, both within psychological formulation, one to one therapy with patients and supervision of the wider multidisciplinary team.
References
Dindo, L., Van Liew, J. R., & Arch, J. J. (2017). Acceptance and Commitment Therapy: A Transdiagnostic Behavioral Intervention for Mental Health and Medical Conditions. Neurotherapeutics. 14 (3), 546–553. https://doi.org/10.1007/s13311-017-0521-3
Graham, C. D., Gouick, J., Krahé, C., & Gillanders, D. (2016). A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clinical Psychology Review. 46, 46–58. https://doi.org/10.1016/j.cpr.2016.04.009
Harris, R. (2009). The House of ACT: Functional Contextualism, ABA and RFT. Book Chapter, 1–23.
Hind, D., Cotter, J., Thake, A., Bradburn, M., Cooper, C., Isaac, C., & House, A. (2014). Cognitive behavioural therapy for the treatment of depression in people with multiple sclerosis: A systematic review and meta-analysis. BMC Psychiatry. 14 (1). https://doi.org/10.1186/1471-244X-14-5
Kangas, M., & McDonald, S. (2011). Is it time to act? The potential of acceptance and commitment therapy for psychological problems following acquired brain injury. Neuropsychological rehabilitation, 21(2), 250–276. https://doi.org/10.1080/09602011.2010.540920
Smith, J. A., Flowers, P., & Larkin, M. (2013). Interpretative Phenomenological Analysis: Theory, Method and Research (Second Ed). http://books.google.com/books?id=WZ2Dqb42exQC&pgis=1
World Health Organization. (2016). What are neurological disorders? Retrieved from: https://www.who.int/news-room/q-a-detail/what-are-neurological-disorders