Written by
Professor Paul van Schaik; Professor of Psychology at Teesside University, Centre for Applied Psychological Science, Cognition and Decision-Making theme. Email: P.Van-Schaik@tees.ac.uk
Late diagnosis of blood-borne viruses remains common in the UK despite national guidelines and other efforts to increase blood-borne virus-testing amongst those at risk of infection. New research in clinical health settings from the Centre for Applied Psychological Science at Teesside University aimed to tackle this health issue. The main idea was to use a computer program that gives an alert in real time to support, prompt and persuade healthcare workers (GPs, nurses and healthcare assistants) to order tests for rare health conditions called blood-borne viruses (BBV): HIV, hepatitis B (HBV) and hepatitis C (HVC). This support is given during consultations with patients where these conditions are not the reason for the consultation. This is important because these conditions are often not picked up in primary care. Based on patient data in the electronic patient record and rules stored in the alert application, ‘BBV Test Prompt’ (https://youtu.be/zS9jLteuT1I/AHSN NENC, 2021; Chadwick, 2018; Chadwick, Forbes & Van Schaik, 2018), the healthcare worker is presented with a blood-borne virus alert within the user interface of the electronic health record system (see Figure 1).
a. Hard prompt – healthcare worker must respond to the prompt before they can continue
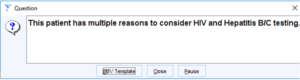
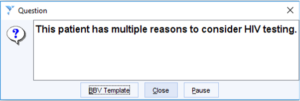
b. Soft prompt – healthcare worker is invited to respond to the prompt, but they can continue even if they ignore the prompt
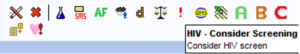
Figure 1 BBV Test Prompt Version 1
Dual-system theory
The effect of such an alert application on healthcare workers’ behaviour can be understood in the framework of dual-system theory (Kahneman, 2011). According to this theory, human thinking (or information-processing more broadly) occurs in two modes: fast and impulsive (System 1), and slow and deliberate (System 2). Much of the time our thinking operates according to System 1 and usually this works well or well enough. However, there are flaws in the way System 1 works, that can sometimes have severe consequences. These problems can be avoided by slow and deliberate thinking (using System 2). However, System 2 has limited capacity, in terms of both the amount of information it can store in memory and the complexity of the computations it can perform to solve a problem. Moreover, System 2 operates according to the law of least effort (System 2 is ‘lazy’); this means that if there are different ways of achieving the same goal, the least demanding path will be chosen. The result is that System 2 is not engaged when perhaps it should be. Therefore, when faced with a more difficult question that requires the use of System 2 (”What are the specific blood-borne virus risk factors to consider for this patient?”), people answer an easier question that System 1 can answer (”What is the first relevant blood-borne virus risk factor that comes to mind for this patient?”). Finally, it is important to note that the two systems do not work independently. For example, information generated or acquired by System 1 may subsequently be used by System 2.
Blood-borne virus alert and dual-system theory
An alert application can reduce the difficulty of identifying patients who should be tested for blood-borne viruses (BBVs): it uses many different factors and rules in a patient’s health record to trigger a BBV alert. For example, BBV Test Prompt Version 1 (BBV_TP1) uses 27 rules and each assesses data on one or more factors from a patient’s electronic health record. However, without an alert application it would be difficult for a healthcare worker to do the required computations themselves, especially in the short space of time that a consultation with a patient in a busy clinic allows. Even if the healthcare worker could do the required computations, they might underestimate the probability that a patient has a higher chance of having a BBV because of a lack of ‘availability’ (the ease with which, for example, HIV/AIDS comes to mind and an example of System 1’s swift but sloppy functioning). This is perhaps because healthcare workers may have rarely encountered a case of HIV/AIDS in their practice, depending on their geography.
The chance that a healthcare worker will follow the alert’s advice to order a BBV test can be increased by the way a problem is presented (this is called ‘framing’), for instance by presenting a pre-set course of action. For example, if the alert presents two options ‘Yes’ (order a BBV test) and ‘No’ (do not order a test), ‘Yes’ is pre-selected. This presentation is justifiable if the rules that the alert system uses are based on strong evidence. Framing the decision with ‘Yes’ as the standard option capitalises on the law of least effort: rather than thinking deliberately about the decision, people tend to choose the suggested course of action – accepting the pre-selected choice. The chance of following the alert’s advice may also be increased by presenting cost-effectiveness information (stating that ordering a BBV test would be cost-effective in the case of the patient at hand) or not presenting information about the previous BBV test that a patient has had (not presenting the date of the last test). This is because both these pieces of information can be used to substitute the original question that System 2 would have to answer (” Should I request a BBV test, considering the collective data in the patient’s health records?”) for an easier question that System 1 can answer (“Would a blood-borne virus test be cost-effective?” or “Has the patient not had a blood-borne virus test recently?”). If the answer to the easier question is ‘Yes’ then the healthcare worker would request a BBV test.
Therefore, critical to the success of an alert application is the way the alert is displayed and how a healthcare worker interacts with it, especially during an appointment with patients. Various studies have identified design factors that are important in the design of such systems and alerts to ensure healthcare workers view the advice, accept it when appropriate and do not succumb to ‘alert fatigue’. From this research, one of the positive predictive factors is quality of display. According to dual-system theory, quality of display increases cognitive ease and makes people’s thinking more effortless (Kahneman, 2011), which may make them more likely to follow the alert’s advice. The frequency of alerts per encounter and repeated reminders may also predict acceptance, although the literature shows mixed evidence for the effect. Familiarity through repeated exposure increases cognitive ease, which – again – makes thinking more effortless, and increases the chance of following the alert’s advice.
Design study of the test prompt
We conducted an online survey experiment with 14 general practices in north-east England (Van Schaik, Lorrimer & Chadwick, 2020) to test the effect of the presentation design of BBV Test Prompt on healthcare workers’ decision-making regarding BBV-testing. Given the importance of healthcare workers’ acceptance of new technology in the workplace, the secondary aim was to determine their acceptance of BBV alerts.
Ten realistic descriptions of hypothetical patients were presented on mock-up screens to healthcare workers who were asked to decide whether to request BBV-testing. The effect of a pre-set course of action to request BBV-testing was significant when additional information (cost-effectiveness, date of last BBV test or risk assessment) was not presented, with a 16% increase from 30% to 46% accept decisions. When risk assessment information was presented without a pre-set course of action, the effects of cost-effectiveness (27% increase) and last test date (23% decrease) were significant. These results are in line with the explanations of behaviour in response to alert presentation given above, based on dual-system theory.
The main reason healthcare workers gave for declining to test was perceived insufficient patient risk of BBV. According to dual-system theory, this may be a case of healthcare workers’ underweighting the probability of disease because of their global impression of frequency of previously experienced cases of BBV. The global impression and therefore the judgement of probability will be (very) low if a healthcare worker has rarely or never seen a case of BBV in their clinical practice. Healthcare workers’ acceptance of the test alert system was high, and resistance was low. We used the results to design a real-world trial of the test alert system.
Testing the blood-borne virus test prompt in general practice
We conducted a second study (Chadwick, Forbes, Lawrence, Lorrimer & Van Schaik, 2021), in which the prototype application (BBV_TP1) was embedded in a primary care electronic health record system. The aim of the research was to establish how effective the application was at increasing the rate of real-time BBV testing and to what extent it was accepted by healthcare workers and patients.
We evaluated BBV_TP1 in 14 general practices in north-east England, in comparison to 54 similar practices that did not use the application. Rates of HIV-, hepatitis B- and hepatitis C-testing in practices were measured before and after the application was activated. Patient and healthcare worker acceptance of the technology was assessed by surveys.
In the six months following implementation of the application, HIV testing rates increased by 556% (from 1.38 to 7.67 per 10,000 patients) and combined HBV/HCV testing rates increased by 361% (from 2.38 to 8.60 per 10,000 patients). No significant differences were observed for any BBV-testing rates in the non-intervention practices over the same period. However, in the intervention practices monthly testing rates declined over time after the large increases. There are two likely reasons for this. First, the trend back to initial testing levels may have been due to reduced engagement by clinicians with the prompt over time: ‘alert fatigue’. Second, it may be that most or all of the patients that would require a BBV test had been tested as a result of the intervention. The decrease in the number of hard prompts (that a healthcare worker must respond to; otherwise, they cannot continue using the electronic health record system) issued after the first 2 months supports the latter reason. Further work is needed to ascertain which of these factors was more important in terms of reduced testing rates.
This study demonstrated that BBV_TP1 increased BBV-testing rates in primary care via targeted screening, providing evidence for the beneficial effect of the alert application by reducing task complexity, although testing rates subsequently fell whilst the application remained active. Such systems can potentially reduce late diagnoses, while having high acceptance by healthcare workers and patients. Larger studies with longer follow-up are needed to demonstrate efficacy and cost-effectiveness.
Conclusion
In conclusion, psychology frameworks such as dual-system theory can help our understanding of how technology, such as a BBV test alert application, can facilitate healthcare workers’ performance. Such frameworks can also help in creating ideas for design and design improvements.
Acknowledgements
I am grateful to the collaborators on this research: David R Chadwick, Sue Lorrimer, Gareth Forbes and Chris Lawrence. Thanks also go to ViiV Healthcare for financial support for the research.
References
AHSN NENC (Academic Health Science Network North East and North Cumbria) (2021). Bright Ideas in Health Awards | Winners Stories – Blood Borne Virus Test (2018). https://www.youtube.com/watch?v=zS9jLteuT1I
Chadwick, D., Forbes, G., Lawrence, C., Lorrimer, S., & Van Schaik, P. (2021). Using an electronic health record alert to prompt blood-borne virus testing in primary care. AIDS, 35(11), 1845-1850.
Chadwick, D. (2018). BBV_TestPrompt. Medipex Innovation Award. Category: Service Improvement – Primary Care. https://www.medipex.co.uk/events/nhs-innovation-awards-2018/
Chadwick, D., Forbes, G. & van Schaik, P. (2018). Blood-borne virus (BBV) test. Bright Ideas in Health Awards. Category: Development of an Innovative Device or Technology. Academic Health Science Network, North East and North Cumbria. https://brightideasinhealth.org.uk/2018-winners/
Kahneman, D. (2011). Thinking, fast and slow. London: Penguin.
Van Schaik, P., Lorrimer, S., & Chadwick, D. (2020). Designing an electronic blood-borne virus risk alert to improve uptake of testing. International journal of STD & AIDS, 31(8), 800-807.